What are Healthcare Restrooms Telling Us?
By Mitch Birchfield
September 29, 2016 | Formats: Article | Content Areas: Environmental Sanitation Operations | Tags: Chemicals , Environmental hygiene and sanitation, Infection Prevention and Epidemiology, Process Improvement
Public or common area health care restrooms need to be thoroughly cleaned and disinfected for user health (due to infection potential on high-touch surfaces) and use touch-less technologies to limit the number of touch point variables and to maximize the effectiveness of cleaning and disinfecting. But they also should be specifically identified and targeted for clean tests and routinely disinfected using supplemental UV light technologies.
Hospital restrooms’ high-touch areas (HTOs) include doorknobs, sink and toilet handles, the toilet seat, handrails, commodes, paper and soap dispensers. Although restroom floors are not hightouch surfaces, they are prone to gross contamination from such things as urine, dirt, and excessive moisture.
Touch-free devices don’t mean that fixtures are not touched; in fact, sensors on faucets and dispensers don’t always activate properly—this means that faucets heads, spigots, and stainless steel including sensors may be contaminated. Additional problems occur with automation; sensors are placed so that flushing occurs much more often than it should or when no one is around. Improperly loaded paper towel dispensers can also be a source of great consternation. Environmental service staffs are rarely asked for their opinions on restroom design features.
For environmental services staffs, cleaning and disinfecting restrooms is overall considered to be one of the toughest areas for service staff to maintain, and paper supply products for dispensers can represent up to 25 percent of an environmental services department budget.
Why focus on public or common restrooms versus patient restrooms?
The sheer volume of uses in public health care restrooms means that surfaces and fixtures can be contaminated, clean and then re- contaminated throughout the day.
Whoever uses the public/common area restroom can contaminate up to seven of the restroom’s high-touch points. which, if not cleaned (and disinfected), can pass an infection to the next user.
Three considerations for cleaning and servicing health care public restrooms:
- Technology Is Simply a Tool to Make Decisions: First is the understanding that restroom technology is a convenience for the users. It isn’t a panacea for making bathrooms cleaner, and logs and indicator tags such as the Awarepoint can be used to alert service staff that bathrooms need attention, and how often certain bathrooms are calling out or alerting us may mean that greater frequencies are needed to service the restrooms, or that the dispensers may be undersized, restrooms vandalized, or paper products removed or stolen.
- Ramp Up to Using Sporicidal Disinfectants: For years, health care facilities have used quaternary disinfectants as “approved disinfectants” vetted by environmental services and infection control professionals as being sufficient to kill most potential infectious materials on surfaces and also safe for surfaces. But the increasing incidence of bacterial and viral infections such as C. diff, MRSA and norovirus has made health care professionals re-assess their cleaning chemical programs.
- Use Resources Wisely—Restroom Service Logs versus Testing and UVing: Do restroom logs offer assurances
that restrooms are well maintained and cleaned? Or are they primarily a customer visual satisfaction tool? In large health care facilities, high volume public restrooms can number over 100, making it a challenge to keep the communications (initial cleanings) current. Additionally, the log becomes of little value if, after cleaning, a customer forgets to flush the toilet, fills up
the trash or sanitary napkin container, or throws paper (toilet or towels) on the floor. In those circumstances, as a Harris poll indicated, customers would view the restroom as dirty; 90, 89, and 80 percent respectively.
A better approach may be to test health care restroom surfaces for cleanliness more regularly, such as using an ATP meter ,and have a routine to use expensive UV devices (beyond patient rooms) to supplement disinfectant efforts, especially considering the number of high-touch surfaces, multiple touches, and other less likely touch areas… such as under dispensers.
So What Exactly Are Health Care Restrooms Telling Us?
It’s one thing if the restaurant or gas station garage isn’t clean, but quite another if a restroom in a health care facility is out of order—not clean, no paper, etc.
When health care organizations recognize that it takes a combination of approaches to keep their restrooms clean, they can then build upon an effective strategy to maintain restrooms at a service level that not only meets the expectations of users but also helps to protect their health.
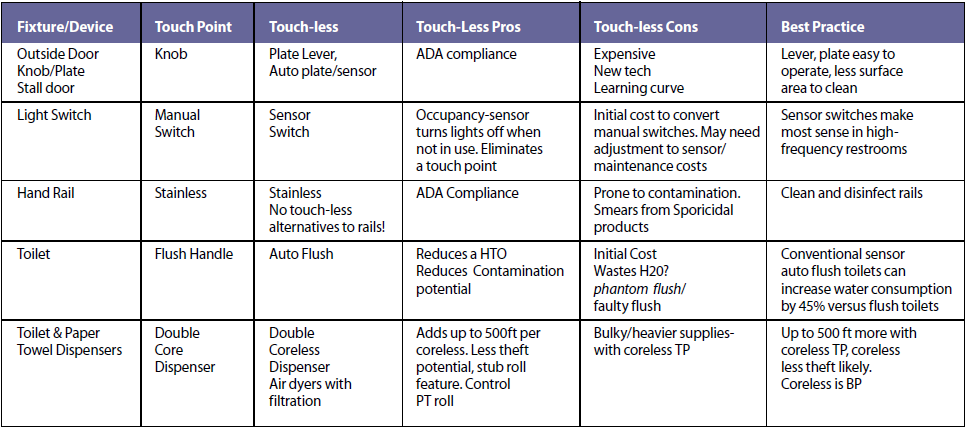
Hospital Restroom Touch Point to Touch List Grid List:
http://www.nxtbook.com/naylor/AHEQ/AHEQ0316/index.php?startid=7#/24

